
Recovery Time
 |
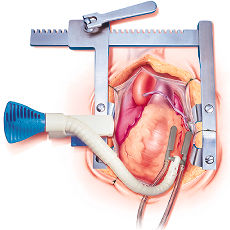
| Figure 10. Beating Heart Surgery Time to Recover |
The anesthesiologists should be an advocate for the patient and must collaborate with the surgeon to allow the patient adequate time to recover between grafts. Although the blood pressure often returns to normal quickly, it may take a longer time for other consequences (such as low SVO2 and acidosis) to resolve. Give the patients more time to recover before another severe hemodynamic insult is produced. If the patient is very sick, the surgeon may elect to perform the proximal grafts prior to the distals. This technique will ensure there is immediate blood flow to that artery upon completion of the distal anastomosis. In addition, it will prevent another potential insult to the ischemic myocardium by placement of the partial occlusion clamp. When the gradient across the partial clamp is measured, it is often in the range of 30 to 50 mm Hg, which may stress an ischemic heart.
Reperfusion
Reperfusion arrhythmias are not common but can occur, particularly in patients who present with unstable angina, e.g., a patient with an unstable clot in a coronary artery. Reperfusion arrhythmias can be severe and require emergent cardioversion. The administration of magnesium or lidocaine before the artery is reperfused can be helpful and should be considered in this situation. Electrolytes should be kept close to normal. Be cautious of administering drugs that are used routinely during conventional CABG procedures, like calcium chloride. A large dose of calcium chloride to a patient who is normo-calcemic can cause heart block. Transient ST segment elevation can occur when the graft is opened and small amounts of air are embolized. In such case the blood pressure needs to be maintained or even increased to "drive" the air through the coronary perfusion system. With this measure the ST changes should resolve, and if they persist, suspicions about a more serious obstruction to coronary blood flow should arise.
 |
| Figure 11. Beating Heart Surgery Reperfusion |
Heparinization
There are diverging opinions among surgeons regarding the amount of heparin to be administered for anticoagulation. Some use modest doses such as 10,000 units while others use traditional doses for bypass (300 to 400 units/kg). There is also divergence of opinion about whether to fully reverse the heparin or not and it is best to ask the surgeon at that time for his or her preference. Generally, an ACT of >250 is recommended.37
Pain Control
Giving a small dose of a non-steroidal agent such as Ketorolac (Toradol®) (15 or 30 mg) in conjunction with lower dose opiates effectively alleviates musculoskeletal pain and avoids the sedation produced by opioids.
Local parasternal infiltration can offer post-operative pain relief (albeit of short duration) after a median sternotomy.
Regional techniques are not very widely used in the US, mainly due to concerns about complications. European physicians suggest that epidural analgesia facilitates the postoperative management, although it is not well established to what extent, and it does carry the risk of an epidural hematoma with a potentially devastating neurological injury.
 |
| Figure 12. Beating Heart Surgery Pain Control |
Extubation
The muscle relaxant should be reversed, the patient should be normothermic, there should not be excessive bleeding, and the hemodynamic parameters should be within normal range before extubation is attempted. We typically do not extubate in the operating room, but rather wait until the patient has been in the recovery room for a short time or in the intensive care unit in order to get a better idea on the amount of bleeding and the patient's temperature. Waiting a short period also gives the patient a chance to become more oriented and able to follow instructions.