
Temperature
Maintaining normothermia is highly desirable. A large portion of the patient's body is included in the surgical field and therefore is not easily warmed. Warming the room can be a helpful intervention but this often results in the discomfort of a heavily gowned operating team performing under hot lights. A sterile forced-air warming device can be placed on the lower body after vein graft harvest and is a useful way to maintain normothermia. The fluids administered can be warmed through a fluid warmer. A heated mattress can also be used. Remember, in light of not having temperature control afforded by CPB, it is much easier to keep a patient warm than to rewarm the patient.
Perfusion Standby
Difficult to expose vessels or conditions such as an intramyocardial coronary may lead to the elective use of cardiopulmonary bypass. CPB may also be needed emergently if the patient becomes hemodynamically unstable or cardiac arrest occurs. Since these events can be unpredictable, the current practice is for the perfusionist and his equipment to be immediately available. The cardiopulmonary bypass circuit can be set up dry so that setup time is minimized in case of an emergency. One report suggests that the perfusion circuit can remain sterile for up to 168 hours wet and three weeks dry when properly covered.29
Ischemia Management
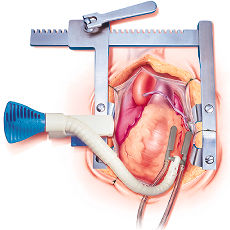
 |
| Figure 4. Beating Heart Surgery: Ischemia Management |
As opposed to conventional CABG, where myocardial ischemia is a potential event, beating heart CAB is characterized by intentional occlusion of specific coronary arteries and virtually certain episodes of regional ischemia. The management of myocardial ischemia requires taking into consideration the myocardial oxygen consumption, myocardial blood supply, tolerance of ischemia, and the monitoring of myocardial status.
Myocardial
Oxygen Consumption
and Control of the Heart Rate
Induction of bradycardia was originally heavily relied on to provide the surgeon with a relatively immobile surface. Stabilization systems have made the induction of bradycardia less important. Despite this, the decrease in the myocardial oxygen consumption that occurs with a decrease in the heart rate is an important benefit for the patient, particularly at a time when supply is compromised. Therefore, the goal remains to avoid marked tachycardia.
If necessary, different drugs can be used to control the heart rate. Beta-blockers are often the first choice, particularly esmolol because of its short duration of action; calcium channel blockers are often used if a radial artery is harvested. Adenosine has been recommended by some as effective to provide an immobile surgical field, but we haven't had to use it with the current tissue stabilization systems. Anticholinergics (such as atropine and scopolamine) should be avoided to prevent tachycardia.
The anesthesiologist should be aware that tachycardia in the context of coronary artery occlusion is often a manifestation of ischemia itself and the response to a low cardiac output. In such a situation, decreasing the heart rate significantly will only further decrease the cardiac output and may lead to hemodynamic instability and/or organ injury.
Ischemic Preconditioning
This concept evolved from experimental data done in Dr. Reimer's laboratory which indicated that 5 minute periods of coronary artery occlusion and reperfusion preceding a long occlusion time markedly decreased the area of myocardial infarction in dogs.30 Other studies31,32 support this concept. While the results in humans have been more controversial, ischemic preconditioning at the very least gives us a glimpse of what the hemodynamic consequences of occluding that particular vessel will be before the surgeon is fully committed.
 |
| Figure 5. Ischemic Preconditioning Ð Size of infarction after occluding a coronary artery for 40 minutes, in dogs. Figure based on data from Murry, et al. 30 |